What is Kidney Failure? Types, Symptoms, Cause, and Treatments
What is Kidney Failure?
Kidney failure means that kidneys no longer filter blood properly, which leads to a buildup of toxins and fluid. When the kidneys fail to perform their function for any reason, kidney failure results. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), end-stage renal disease (ESRD) is when kidneys function at less than 10-15% of their normal capacity. This functioning level refers to the glomerular filtration rate (GFR), a key indicator used to diagnose end-stage renal disease (ESRD).
What if you have one working kidney?
The kidneys work together, but they don't strictly divide their function into 50% each. They collectively perform the body's filtration needs. If one kidney is removed, the remaining kidney can enlarge and compensate to meet the body's needs.
The leading causes of kidney failure include uncontrolled diabetes, persistent high blood pressure, and kidney injuries. It also increases the rate of heart disease and stroke in renal patients.
When both kidneys fail, it leads to fluid retention, electrolyte imbalances, high blood pressure, anaemia, bone health issues, uremia, heart disease, gastrointestinal problems, decreased immune function, and cognitive impairments. Nausea, vomiting, fatigue, frequent urination, and swelling of body parts are some symptoms of kidney failure. The severity of symptoms depends on whether they are acute or chronic.
Acute kidney injury (AKI), also known as acute renal failure, develops quickly and is treatable. It can be caused by any infection, blood loss due to major injury, or excessive use of some medicines. In severe cases, if left untreated, acute kidney injury can progress to permanent damage or even progress to chronic kidney disease.
Chronic kidney disease (CKD) is a long-term condition that may slowly get worse. It is mainly caused by high blood pressure, or diabetes, which slowly damages the kidneys and decreases their function over time.
Types of Kidney Failure
There are 2 major types of kidney failure, depending on their severity, causes, and factors. These include acute kidney failure and chronic kidney failure, which are further subdivided into the following categories.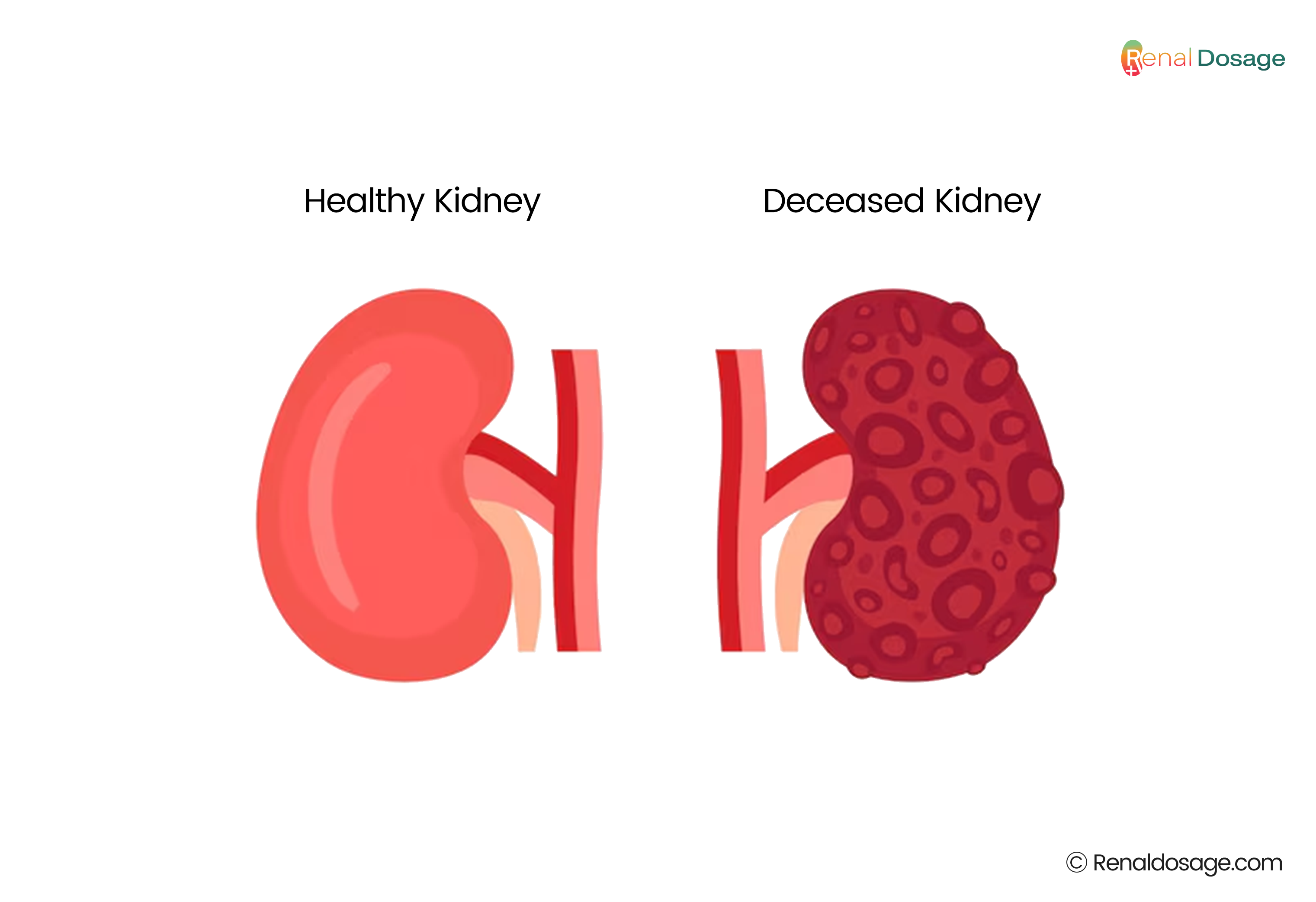
-
Acute Prerenal Kidney Failure
Acute prerenal kidney failure is caused by insufficient blood supply to the kidneys. Doctors can treat it by determining the cause of decreased blood flow. -
Chronic Prerenal Kidney Failure
Chronic prerenal kidney failure occurs when there is insufficient blood supply to the kidneys for a longer period of time. In this condition, the kidneys shrink and lose the ability to perform their function. -
Acute Intrinsic Kidney Failure
Acute intrinsic kidney failure occurs due to direct trauma to the kidneys. It may be due to physical impact, accident, excessive toxins or ischemia. The term ischemia refers to the deficiency of oxygen in the kidneys. -
Acute Post-renal Kidney Failure
The temporary blockage in the urinary tract and kidney stones are the main reasons for acute post-renal kidney failure. -
Chronic Post-renal Kidney Failure
The long-term blockage in the urinary tract can cause chronic post-renal kidney failure. It results in obstruction of urination caused by high pressure and eventually leads to kidney diseases.
What are the early signs and advanced symptoms of kidney failure?
Kidney failure doesn't show noticeable symptoms at the early stages. According to the Centres for Disease Control and Prevention (CDC), about 90% of people are unaware that they are suffering from kidney diseases. The early-stage symptoms of kidney failure include:
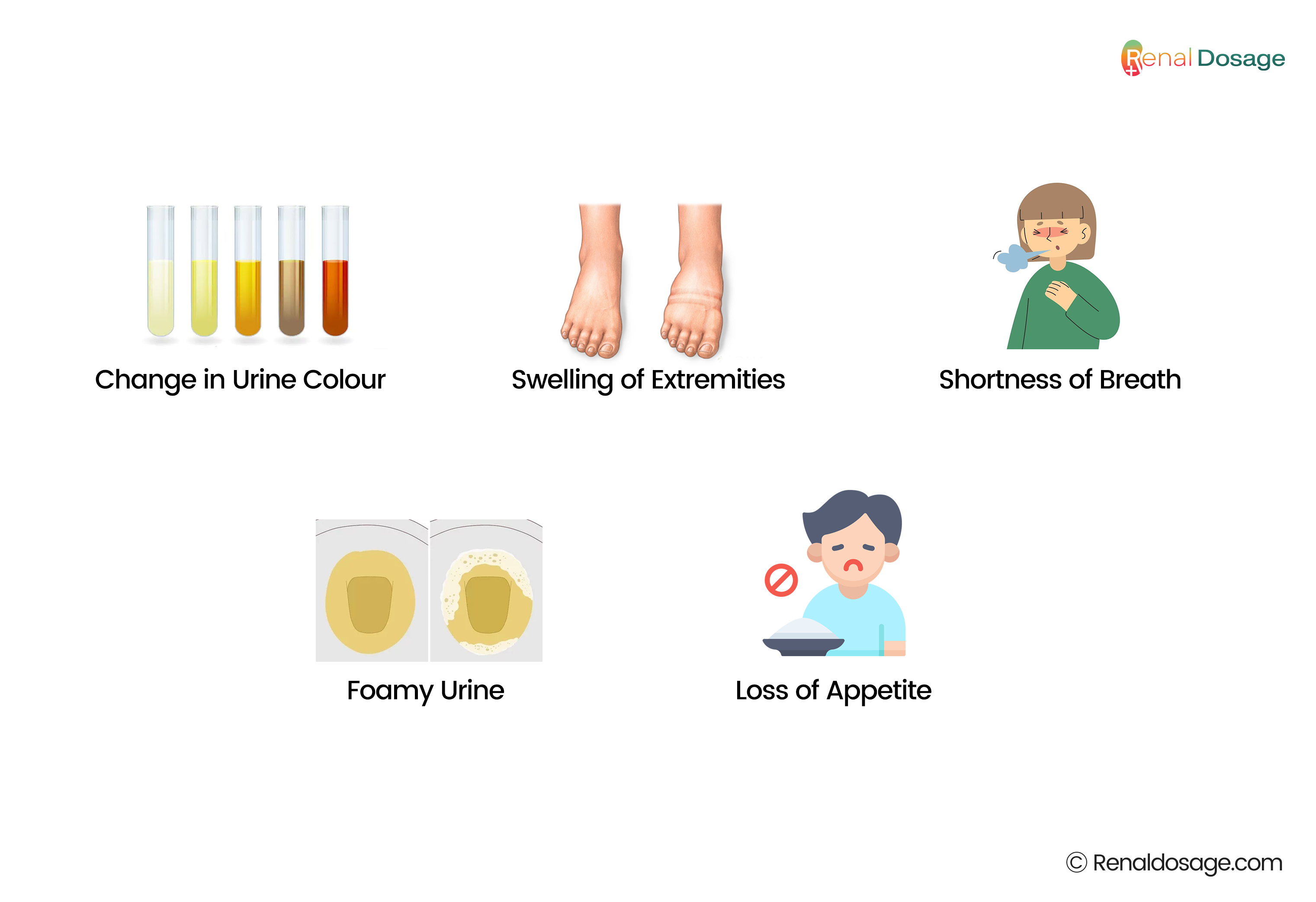
- Low urine output and change in urine colour
- Swelling of extremities (oedema)
- shortness of breath
- Foamy urine (from proteinuria)
- Loss of appetite.
There are 8 severe symptoms of kidney failure, including
- Muscle cramps during the night
- Difficulty in sleep
- Fatigue and drowsiness
- Persistent nausea
- Confusion
- Chest pain
- Seizures
- Coma
Complications of Chronic Kidney Disease
These are severe complications and health risks of kidney failure. It includes
- Anaemia
- Bone weakness (deficiency of phosphorus and calcium)
- Fluid retention (oedema)
- Hyperphosphatemia (a condition in which you have too much phosphate in your blood.) often leads to secondary hyperparathyroidism ( increase in parathyroid hormone levels in the blood.)
- Low immune response
- Sexual dysfunction
- Cardiac disease
- Increased potassium levels (hyperkalaemia)
- Metabolic acidosis ( is when acids build up in your body.)
These symptoms also lead to secondary complications with kidney failure. It includes:
- Gout
- Depression
- Liver failure
- Skin infections
- Nerve damage
- Fluid buildup in the lungs
They disrupt routine activities and reduce quality of life. To manage these complications properly, lifestyle changes, frequent medical appointments, and potential dietary restrictions should be improved. Lifestyle changes involve a healthy diet, exercise, and proper medications to manage complications like fluid retention and electrolyte imbalances.
What Causes Kidney Failure or Dysfunction?
According to the National Kidney Foundation, the two most common causes of kidney failure are high blood pressure and diabetes.
- Diabetes: Uncontrolled diabetes can lead to high blood sugar levels (hyperglycemia). Persistent high blood sugar can damage kidneys and other organs. High blood sugar causes the glomeruli to become thickened and scarred, which reduces the ability to filter effectively.
This damage is called diabetic nephropathy. It also results in an increase in pressure within the glomeruli, known as glomerular hypertension. This increased pressure causes further damage to the delicate filtering structures. - Hypertension: High blood pressure forces blood through the vessels at a higher-than-normal pressure, causing the walls of the blood vessels in the kidneys to thicken and narrow. This restricts blood flow, reducing the kidneys' ability to filter blood effectively.
The increased pressure and reduced blood flow lead to glomerulosclerosis, a condition in which the kidney’s glomeruli become scarred and lose their ability to filter waste from the blood. If left untreated, it results in kidney failure.
Causes of Acute Kidney Failure
Acute kidney failure, or acute kidney injury (AKI), is a condition in which blood flow to the kidneys decreases for any reason. It is a reversible disease that can be treated with precautions and treatment. If left untreated, it progresses to chronic kidney disease.
Some external factors, like drug toxicity, can also contribute to renal failure. Some causes of acute kidney failure are
- Kidney injury or inflammation due to accident
- Blockage in the urinary tract due to prostate, colon, or cervical cancer
- Loss of blood flow due to injury, burn, dehydration, or allergic reactions
Causes of Chronic Kidney Failure
Besides hypertension and diabetes, the other causes of chronic kidney diseases include
- Polycystic kidney disease (PKD) - a genetic disorder with the formation of many cysts in the kidneys,
- A severe, long-term kidney infection
- Autoimmune diseases
- Prolonged obstruction of the urinary tract
- Vasculitis
- Intake of toxic drug
- IgA glomerulonephritis
- Heavy metal poisoning, such as lead
- Alport syndrome (a rare genetic condition)
- Haemolytic uremic syndrome in children
- Stenosis of renal artery
- Myeloma - a cancer of the plasma cells in bone marrow
- Scleroderma - an autoimmune condition that affects the skin
- Thrombocytopenic purpura - a disorder that causes blood clots in small vessels
TO READ MORE ABOUT POLYCYSTIC KIDNEY DISEASE
Who Faces Kidney Failure?
People of all ages are prone to kidney diseases, but this risk increases with age. According to the Centres for Disease Control and Prevention (CDC), about 14% of adults in the total population of the U.S. suffer from chronic kidney failure. People with diabetes, high blood pressure, heart disease, a family history of kidney failure, abnormal kidney structure, and over the age of 60 are more likely to have kidney failure in the future. According to research in the U.S., it is reported that about 750,000 people suffer from kidney failure each year, which affects 2 million people worldwide.
Stages of Chronic Kidney Disease
Depending on the eGFR values, kidney diseases are classified into five stages. These range from very mild (stage 1) to complete kidney failure (stage 5). As the value of eGFR decreases, symptoms and complications increase as the stages progress.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), approximately 1 in 500 Americans has stage 5 kidney failure.
|
Stages |
eGFR value (mL/min/1.73 m²) |
Complication |
Symptoms |
|
Stage 1 |
Higher than 90 |
No visible complications |
No symptoms |
|
Stage 2 |
60- 89 |
Mild infection |
Protein in the urine |
|
Stage 3 |
30- 59 |
Cardiovascular disease |
Swelling in hands and feet |
|
Stage 4 |
15- 29 |
Hyperkalaemia |
Anaemia |
|
Stage 5 |
Below 15 |
Complete kidney failure |
Loss of kidney function |
Diagnosis and tests of Kidney failure?
It is very important to diagnose the condition properly before starting treatment. To diagnose kidney health conditions, doctors recommend the following common tests:
- Blood samples: Blood tests aid in diagnosing the condition and measure substances filtered by the kidneys. Blood tests include blood urea nitrogen (BUN) and serum creatinine. Increases in BUN and creatinine levels indicate acute kidney failure.
- Urinalysis: In urinalysis, a urine sample is taken to detect various substances, including protein (proteinuria) and sugar (glucosuria). The presence of an excess amount of protein in urine indicates kidney disease or damage. Conditions like diabetes or hypertension can lead to proteinuria before kidney failure occurs. Excess sugar in the urine indicates uncontrolled diabetes that can lead to kidney damage over time.
- A urinary sediment examination (solid particles found in the urine after centrifugation) looks for red and white blood cells, high levels of bacteria, and high numbers of cellular casts. Red blood cells in urine indicate bleeding within the urinary tract, while white blood cells and bacteria refer to infection (urinary tract infection). The presence of a cast in urine indicates kidney damage. Cellular casts are microscopic cylindrical structures found in urine, often indicative of kidney disease (such as red or white blood cell casts).
- The urine albumin-creatinine ratio (uACR) test detects early symptoms of kidney damage. It is an important diagnostic tool used in urinalysis to assess kidney function. It measures the amount of albumin relative to creatinine in a urine sample.
- Imaging: Imaging tests also help diagnose kidney-related problems. Ultrasounds, MRIs, and CT scans provide images of the kidneys and urinary tract, helping to identify the main issue of kidney failure.
- Kidney Biopsy: A kidney biopsy involves removing a small piece of kidney tissue to examine under a microscope. It helps doctors investigate the cause of kidney damage and failure.
Treatment and Management of Kidney Failure
-
Dialysis
Dialysis is the most common method of treating kidney diseases. It involves a dialyser machine to filter and purify the blood. There are two types of dialysis. The type of treatment depends on the stage and severity of kidney diseases. During dialysis, a person is recommended to take a low-potassium and low-salt diet.
- Haemodialysis
- Peritoneal Dialysis
-
Haemodialysis

In haemodialysis, blood is passed through a machine called a dialyzer. The dialyser cleans and filters the blood and returns the purified blood back to the body. This machine regularly cleans your blood. It is usually done 3 times a week at the hospital or dialysis centre. Blood is entered from the body, cleaned by the machine, and then returned to the body.
During a haemodialysis session, needles are placed in a blood vessel, often in the arm. Each session lasts about 3-4 hours and is usually performed at a dialysis centre. Haemodialysis is effective for removing waste and allows for more regular monitoring of health. -
Peritoneal Dialysis
Peritoneal dialysis uses the abdomen’s lining to filter the blood. A special fluid is used to absorb waste from the blood. In peritoneal dialysis, a catheter is placed into the abdomen. Through this catheter, a fluid called dialysate is introduced. Waste and extra fluid from the blood move into the dialysate. After a few hours, the used fluid is drained and replaced with fresh fluid. This process can be done manually several times a day or automatically using a machine while sleeping. Peritoneal dialysis can be done at home, which offers flexibility and convenience. It also provides a more continuous form of treatment.
-
Kidney Transplant
Kidney replacement is another option for treating damaged kidneys. It is a common treatment for end-stage renal disease. A kidney transplant is a method of replacing a damaged kidney with a healthy one. A transplanted kidney does not require dialysis. There’s usually a long wait to receive a donor kidney that’s compatible with the patient’s body. The process goes quickly if the patient finds a living donor.
While kidney transplants have risks, they are generally very successful for the right candidates and can significantly improve life expectancy and quality of life. Patients need to take immunosuppressant drugs for a longer period of time after the surgery for kidney acceptance. They have side effects, but most are manageable. While transplants carry risks, they are generally very successful and can significantly improve the quality of life for those who are eligible.
Kidney Transplant Recovery:
- Possibility of Kidney Rejection: When a person is given a kidney transplant, there is always a possibility of the body rejecting the transplanted organ. This may happen right after the surgery or several years later. In order to avoid rejection, the patient is given immunosuppressive drugs that they must continue taking for the rest of their life.
- Ongoing Monitoring: It is important to have follow-up visits after the kidney transplant. A person will have to undergo blood and urine testing, along with other tests, to evaluate the performance of the transplanted kidney and look for signs of rejection or other problems.
- Long-Term Survival Rates and Quality of Life: Most patients who have had kidney transplants described positive changes in their quality of life. Improved health, better physical well-being, increased energy levels, and the ability to perform normal activities are observed. The long-term survival rates are also well proportional in transplanted kidneys and have shown efficient results for 10-20 years or even more. Life expectancy depends upon factors like age, the health status of the patient, and compliance with medication.
Can I recover from kidney failure?
Yes, a person can recover from kidney failure with proper treatment. The treatment and recovery depend on the severity of renal disease. Recovery from acute kidney injury is possible and can lead to a full restoration of kidney function. Chronic kidney failure requires ongoing treatment and management to maintain health and prevent further deterioration of kidney damage. A person with chronic renal failure requires treatment for the rest of their life.
How long can you live with kidney failure?
It is not possible to measure the life expectancy of a person with renal disease, as it depends on several factors.
- Age
- The main cause of renal diseases
- How well that underlying cause is managed
- Other complicating factors, like high blood pressure or uncontrolled diabetes
- Stage of kidney disease at diagnosis
According to the National Kidney Foundation, it is reported that a person on dialysis can live 5-10 years as long as treatment. Some people can also live more than 20 to 30 years, depending on the tolerance level and health conditions.
At end-stage renal failure, missing one dialysis treatment decreases life expectancy. Without proper treatment, dialysis, or a kidney transplant, a person can survive a few days or weeks without treatment. The average life expectancy with a kidney transplant from a living donor is 12 to 20 years and from a deceased donor is 8 to 12 years.
What medications are used to treat kidney failure?
Doctors prescribe medications according to the severity of complications and symptoms of renal failure. The following medicines are commonly prescribed to treat renal failure and its complications.
- Angiotensin-converting enzyme (ACE) inhibitor or angiotensin II receptor blocker (ARB): This medication decreases blood pressure, is beneficial for hypertensive patients, and protects kidney function.
- Diuretics: These help remove extra fluid from the body and ensure the maintenance of blood pressure.
- Statins. These medications lower cholesterol levels and are beneficial for hypercholesterolaemia patients.
- Erythropoietin-stimulating agents: These help build red blood cells and are advantageous to anaemic patients.
- Vitamin D and calcitriol. These help prevent bone loss.
- Phosphate binders: These help remove extra phosphorus in the blood.
What not to drink if you have kidney problems?
If someone is suffering from renal problems, it's important to avoid or limit certain beverages. These drinks can further stress the kidneys or worsen the overall condition. Here are some drinks to avoid:
- Limit sodium and potassium: It is recommended that sodium and potassium intake be less than 2000 mg per day. This includes fruit juices, energy drinks, coffee or caffeinated drinks, sports drinks and sugary beverages.
- Limiting phosphorus: Renal patients should consume less than 1,000 milligrams of phosphorus per day. The amount of phosphorus is present in some drinks, colas and processed beverages. For example, milk is high in phosphorus and potassium and is limited in kidney disease.
- Protein guidelines: In the early stages, protein restriction might be recommended to reduce kidney workload, but protein intake might need to be managed differently in end-stage kidney disease.
- Restricting alcohol intake: Alcohol intake is strictly restricted to renal patients because it doesn't metabolise out of the system. If the kidneys don't filter alcohol from blood, it causes severe complications and even death.
What foods support kidney Function?
It's essential to maintain a well-balanced diet that is high in vitamins and nutrients and low in sodium. Many fruits and vegetables help kidney functions. These foods support kidney health by reducing strain on the kidneys and promoting overall health. Healthy habits and routines slow down kidney progression disease.
Fruits that are rich in vitamin C help in supporting damaged kidneys. They are superfoods that include pomegranates, strawberries, blueberries, apples, cherries, and acai berries. Foods that are low in sodium, potassium, and phosphorus are beneficial in renal disease patients. Other foods that are beneficial for kidney health are
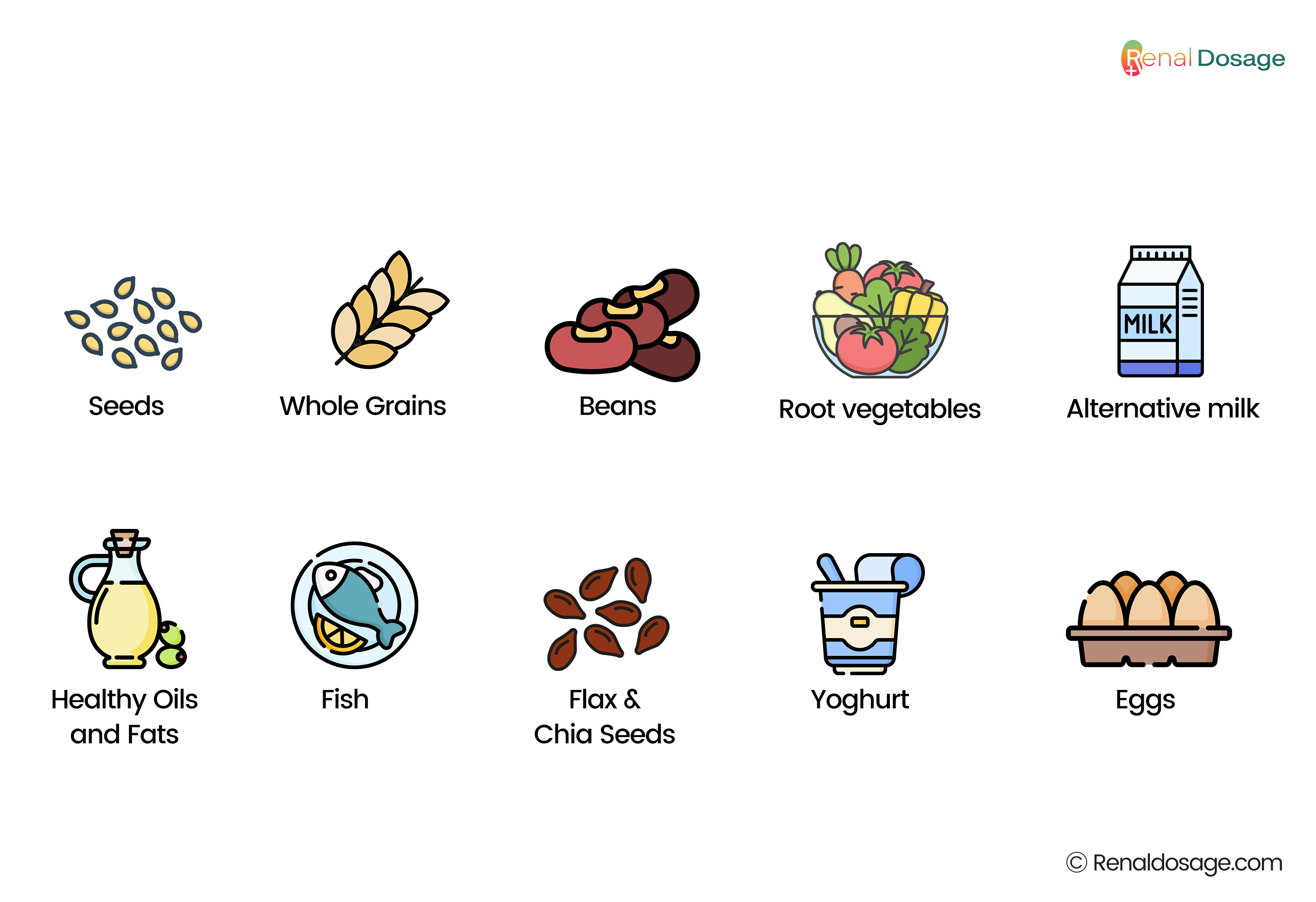
- Seeds
- Whole grains
- Beans
- Root vegetables such as carrots and onions
- Alternative milk (vs. cow milk)
- Healthy oils and fats
- Fish
- Flax and chia seeds
- Yoghurt
- Eggs
Importance of Hydration with Water
Water is a basic necessity of life. It is very important in supporting other body functions. Water is needed to regulate physiological functions such as movements, brain and skin functions, and digestion. Normal adults are advised to drink 8-12 glasses of water daily.
However, the volume of fluid intake depends on the kidney's health status for the disease. There is an enhanced water intake in kidney stones and a reduced intake in patients under dialysis. Water is essential to meet the body’s needs for hydration.
- Improving physical performance
- Boosts cognitive function
- Aids in digestion and detoxification
- Promotes healthy skin
- Helps in weight management
- Maintains cardiovascular health
To obtain the necessary fluids, it is necessary to drink water in the morning, half an hour before meals, during mealtime, after physical activity, and before going to bed. Taking a glass of water before half an hour of meals aids digestion and avoids the consumption of excess food. Consuming water and electrolytes after exercise allows the body to recover fluids and salts lost during sweating.
How can I prevent kidney failure?
It is important to follow these steps to prevent kidney failure. These points are recommended as healthy measures and practices to prevent the advancement of kidney disease.
- Monitor the functioning of kidneys.
- Control blood sugar level in the normal range.
- Maintains blood pressure levels in a normal range.
- Avoid smoking, alcohol, and tobacco products.
- Follow a healthy meal plan.
- Maintain balance weight
- Avoid NSAIDs and OTC medications.
- Avoid foods high in protein, potassium, phosphorus, and sodium.
- Follow-up with a healthcare provider.
Advancements in Kidney Health Research and Treatment
Latest Research
Kidney health research has seen significant advancements in recent years, leading to improved treatment options and innovative management strategies for kidney disease. Some of the notable advancements include:
Regenerative Medicine and Stem Cell Therapy
Kidney diseases are becoming a major public health issue. Chronic kidney disease (CKD) has detrimental effects on human health. Researchers are currently exploring the possibility of using stem cells to recover damaged kidney tissue. Early-stage clinical trials have shown effective results in some patients with partial kidney function restoration.
Stem cells are organs that can self-renew and adopt other cell functions. They are essential in replacing damaged tissues in the kidney and enhancing overall kidney performance.
Recent research has shown that stem cells are beneficial in the treatment of acute and chronic kidney diseases. The cells can recover damaged organs and encourage normal healing processes in the body. Stem cell therapy is safe and within reasonable tolerance in initial human clinical trials.
Scientists are studying various types of stem cells and their mechanisms to treat damaged kidneys. This research is useful as it identifies the strengths of utilising stem cells for the treatment of kidney disease while recognising its limitations and the need for further study in the field.
Future Outlook
Advanced technologies, including regenerative medicine(RM) and new therapies in kidney health and treatment options, are creating further improvements. According to research by Astgik Petrosyan1, published in Frontiers in Bioengineering and Biotechnology, regenerative medicine technologies are used in transplant medicine.
The upcoming treatment solutions for kidney diseases can be traced to the field of regenerative medicine (RM). This field aims to look for methods to heal or rebuild injured tissues or organs, particularly kidneys in renal diseases.
New therapies are evolving by merging transplant medicine with other approaches to regenerative medicine, which is creating personalised treatments. These include innovative tools like cell-based therapies, tissue engineering, and the use of special materials to help rebuild organs.
This approach is especially beneficial for kidney diseases because it may offer a chance to regenerate damaged kidneys or build new ones for transplants. It offers a long-term solution to damaged organs and reduces the dependency on organ transplants and dialysis.